Self-awareness
The successful alleviation of the clinical consequences of acquired brain injury depends not only on their intensity, but also on their level of self-awareness.1 Impaired self-awareness has been defined as a reduced ability to appraise one’s strengths and weaknesses and the implications for daily life activities at present and in the future. Self-awareness is a broad and complex concept that imply the interaction of different cognitive processes and primary human psychological functions. As a proof of its complexity, there is no consensus of the neural signatures of this ability. Although impairments of self-awareness were preliminary linked to frontal lobe, recent studies suggest that they may result from breakdown of functional interactions between nodes within the fronto-parietal control network.
Self-awareness deficits can have serious implications for everyday functioning. They can make patients not understand the purpose of their participation in a neurorehabilitation program, and, in consequence, patients can present lack of motivation and cooperation, and even irritability. They can also lead patients to set unrealistic goals, thus complicating their everyday functional competence, and vocational reentry. In addition, impairments in emotional self-awareness can affect the understanding of the differences between oneself and others, the adaptation to another’s perspective, and the modulation of the behavior to other’s reactions. Consequently, self-awareness deficits can have a special impact on social skills and emotional regulation, which can make community integration difficult.
Group therapy with a game board
Different strategies have been proposed to improve impairments in self-awareness. Many studies have explored the effectiveness of behavioral interventions, confrontational techniques, motivational interviews, counseling, and psychotherapy. Interventions commonly incorporate feedback of performance of tasks, whether verbally by a therapist or visually by previous videotaped sessions. Interestingly, educational formats have shown to help understanding of the residual impairments and their implications, which can be promoted by group therapy programs, even using game-based approaches. However, although the promising results after group interventions, little research has been done on the interactions between SA and social skills.
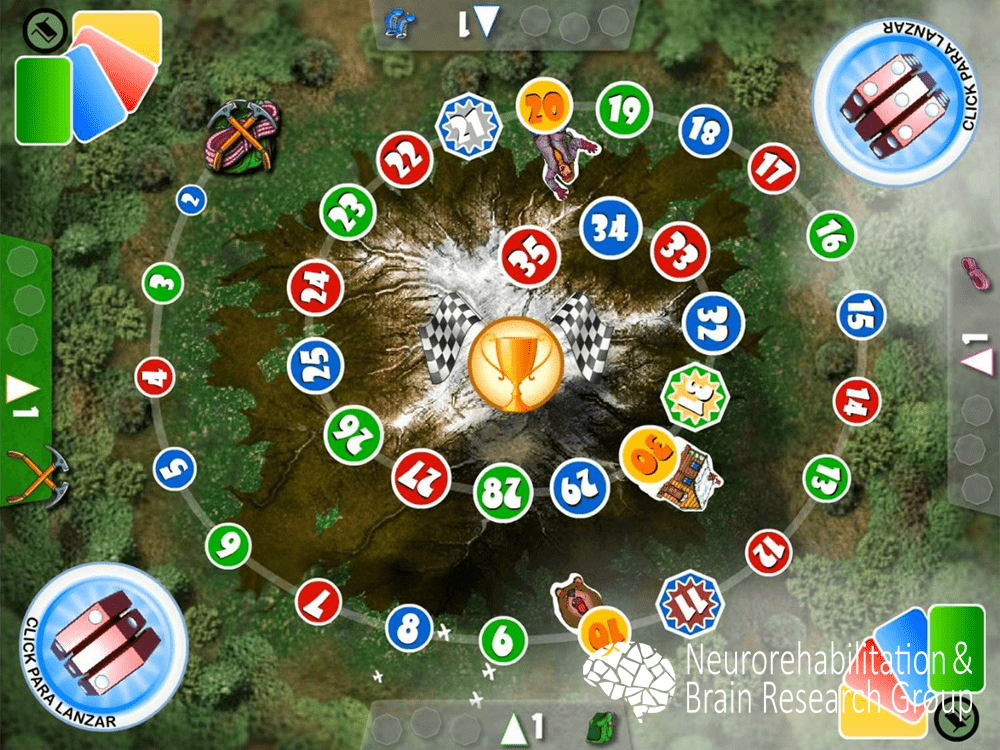
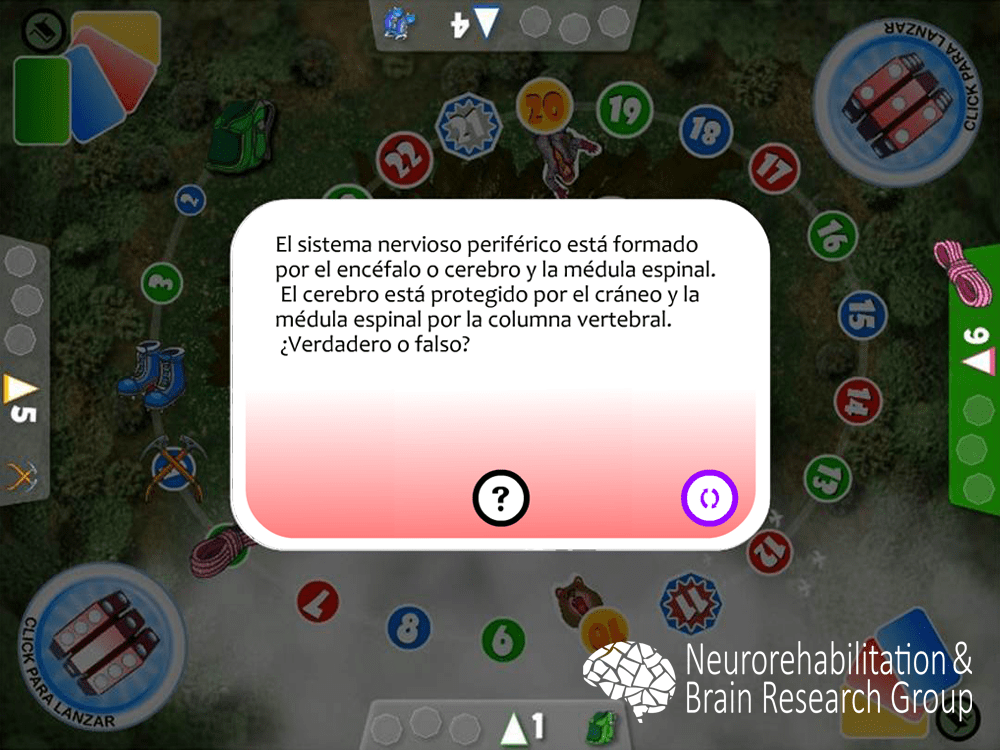
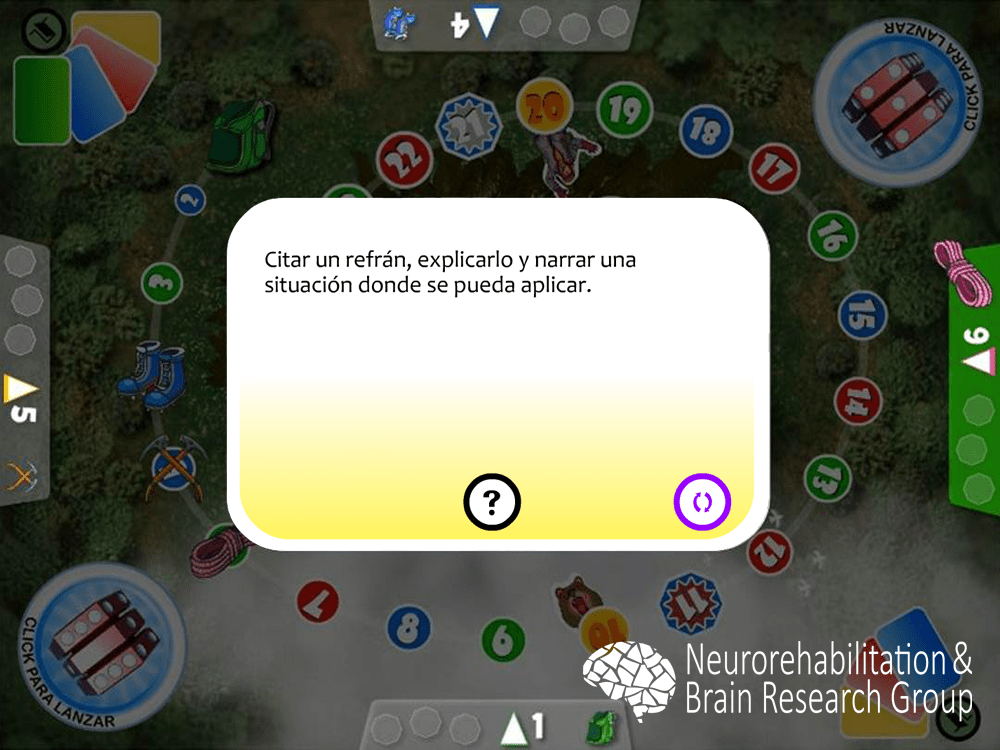
We developed a game-based group therapy that focuses on social interaction to improve self-awareness. During the intervention, participants are divided into groups of two people that present similar cognitive conditions and play a customized game board, which represents a mountain climbing. Each team strove to reach the summit first by correctly answering questions presented on cards as fast as possible. Question cards included four different types of questions: knowledge (anatomical and pathological matters), reasoning (situational exercises), action (role-playing exercises), and cohesion (jokes and sayings).

Group therapy with a multitouch tabletop system
More recently, we have developed a multitouch tabletop system that provides augmented audiovisual feedback, improves the management of participants, and register the results. A multi-touch screen was embedded into a conventional table to display the game board. Participants engage by touching elements presented on the screen.
Interventions involving the tabletop system provided similar effects to those with the game board. Pilot studies involving individuals with acquired brain injury confirmed the improvement in the perception of deficits and disability and their plan-making, and evidenced an improvement in the social skills, which could be derived from the group therapy.3 In addition, the differences in the perception of deficits between patients and their relatives and frontal systems behavioral syndromes decreased after the intervention.4
When only subjects with traumatic brain injury were enrolled, the experimental intervention supported previous results in acquired brain injury population, showing an improvement in perceptions of deficits, of their implications, and of long-term planning, and on the social skills and behavior.5 These results are specially interesting due to the high incidence of these deficits after traumatic injuries, ranging from 45% to 97% of the cases, which could be derived from the diffuse neuroanatomical distribution of the self-awareness neural network that makes it extraordinary vulnerable to diffuse axonal injury.
Participant self-reports exhibited strong program acceptance. Subjects reported high levels of interest and enjoyment, found themselves competent but not pressured, and considered the intervention useful. In addition, they deemed the system highly accessible.4,5
References
- Noé E., Ferri J., Caballero M.C., Villodre R., Sánchez A., Chirivella J. (2005). Self-awareness after acquired brain injury: predictors and rehabilitation. Journal of Neurology, 252(2):168-75.
- Caballero C., Ferri J., García M.C., Chirivella J., Renau O, Ferri N., Noé E. (2007). Escalada de la conciencia. Un instrumento para mejorar la conciencia de enfermedad en pacientes con daño cerebral adquirido. Revista de Neurología, 44(6): 334-338.
- Llorens R., Navarro M.D., Alcañiz M., Noé E. (2012) Therapeutic effectiveness of a virtual reality game in self-awareness after acquired brain injury. Studies in Health Technology and Informatics. 181:297-301.
- Llorens R., Alcañiz M., Navarro M.D., Ferri J. (2013) Self-awareness rehabilitation through a multi-touch virtual game board after acquired brain injury. International Conference on Virtual Rehabilitation 2013, 134-138.
- Llorens R., Noé E., Ferri J., Alcañiz M. (2015) Videogame-based group therapy to improve self-awareness and social skills after traumatic brain injury. Journal of NeuroEngineering and Rehabilitation. 12: 37.